45 Year old man lost in his own thoughts for 20 years and recurrent left hemiparesis for three days
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
45year old male who came from *** is a tailor by occupation married for 20years with a son and a daughter came with chief complaints of weakness of left upper limb and lower-limb with deviation of mouth and slurring of speech since 3 days
Patient was apparently asymptomatic 20years back then attenders of the patient noticed altered behaviour in patient with decreased attention span. The patient is lost in his own thoughts even while he is speaking and they also noticed that he started speaking to himself. He has not taken any treatment for it.
Then 3years back then he developed fever which was lasting for a week associated with cough with expectoration for 2 weeks. He was taken to government hospital where he was diagnosed with pulmonary koch’s for which he received treatment for 6 months. After completion of treatment, he gives no history of testing negative for koch’s. He also gives history of pleural tapping done during his stay in the hospital.
Then 3 days back he had giddiness around 6pm while he was doing plaster work for walls ( which he does occasionally since 4 years). At that time he was lifting weights and suddenly had giddiness and sat down for 2-3 mins. As he was not able to get up on his own, his son and the people around him have taken him back home where he was found out to be having low blood pressure by RMP. He also noticed that ? he could not lift left upper limb and lower limb and there was deviation of mouth to right side. Slurring of speech was present.
There were 3 similar episodes of giddiness lasting for 2-3 mins followed by weakness of left upper limb and lower limb after the first episode. After the episodes he was able to regain back his normal functions. He was able to perceive smell, taste and his vision was normal. There was no loss of sensation of face. He was able to chew food, button and unbutton his shirt, hold objects and catch hold of things which were over the shelf.
No H/o pain in the calf muscles while walking/calf tender positive.
No H/o difficulty in standing from sitting position.
No H/o difficulty in climbing stairs
No H/o difficulty in holding chappals
No H/o wasting and thinning of muscles (LL>UL)
No h/o difficulty in getting up from lying down.
no h/o difficulty in holding pen/ buttoning/ unbottoning
no h/o difficulty in breathing
no h/o difficulty in lifting the head off the pillow
no h/o difficulty to roll over the bed
no h/o involuntary muscles
no h/o fasciculations/muscle twitchings
No h/o slippage of chappal while walking without knowledge
no h/o sensory deficit in feeling clothes
no h/o sensory deficit for hot/cold
no h/o tingling and numbness in UL & LL
no h/o band like sensation
no h/o low backache
no h/o trauma
no h/o giddiness while washing face
no h/o cotton wool sensation
no h/o urgency/hesitancy/increased frequency of urine
no h/o urinary incontinence
No h/o nausea/ vomiting/diarrhea
no h/o seizures
no h/o spine disturbances
no h/o head trauma
no h/o loss of memory
no h/o abnormality in perception of smell
no h/o blurring of vision
no h/o double vision/difficulty in eye movements
no h/o abnormal sensation of face
no h/o difficulty in chewing food
no h/o difficulty in closing eyes
no h/o drooling of saliva
no h/o giddiness/swaying
no h/o difficulty in swallowing
no h/o dysphagia/dysphasia
no h/o tongue deviation
no h/o difficulty in reaching objects
no h/o tremors/tongue fasciculations
no h/o incoordination during drinking water
no h/o fever/neck stiffness
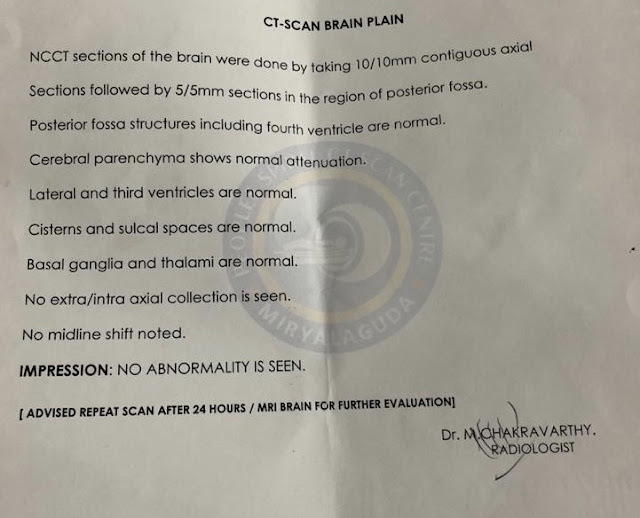
Then on next day he was taken to a hospital near to his place. He was having left sided weakness during his visit to hospital. At that hospital CT brain and other tests were done. CT brain showed no abnormality. He was found to be having low serum potassium for which syrup Potchlor was given. He was almost recovered.
He was referred to our hospital in view of better management
When the patient presented to the casuality, he had no loss of weakness of left upper limb ,lower limb and no deviation of mouth. Slurring of speech was not present.
He gives history of toddy consumption occasionally and consumption of brandy and whiskey every alternate day since 20years. H/O chewing of chauni (tobacco) one packet daily since 10years.
He has a mixed diet with normal appetite and normal bowel and bladder movements.
Not a known case of diabetes, hypertension, cerebro vascular accident , coronary artery disease.
GENERAL EXAMINATION:
Thin built and moderately nourished
NoPallor, icterus, cyanosis, clubbing, lymphadenopathy, Edema.
no short neck
no scars;no h/o tropic ulcers
no neurocutaneous markers
Afebrile
Bp -120/70 mmhg
Pulse-80 bpm
RR- 17cpm
SYSTEMIC EXAMINATION
CVS- s1 s2 heard no murmurs
RESPIRATORY SYSTEM -bilateral air entry present , + normal vesicular breath sounds. no added sounds.Traches central in position
PER ABDOMEN-
Scaphoid in shape,no tenderness and no palpable mass present.Hernial orifices are free.Liver and spleen are not palpable.Bowel sounds are present.
CNS:
Higher motor funtions normal
patient is conscious and oriented to place/time/person
MMSE- 26
Pt has decreased attention span and doesn't respond when sometimes questions were asked.
All cranial nerves- intact
MOTOR SYSTEM
Right Left
Bulk: inspection Normal Normal
palpation. Normal Normal
Measurements U/L Equal on both sides
L/L Equal on both sides
Tone:
UL Normal Increased
LL Normal Normal
Power :
UL 5/5 5/5
LL 4+/5 4+/5
Reflexes: absent
SENSORY SYSTEM
RIGHT. LEFT
SPINOTHALAMIC
crude touch. N. N
pain. N. N
temperature. N. N
post:
fine touch. N. N
vibration. N. N
position sensor. N. N
cortical
2 point discrimination N. N
tactile localisation. N. N
CEREBELLAR SIGNS - normal
No meningeal signs
Outside CT report
PSYCHIATRY REFERRAL WAS DONE
DAY 1 at 11:30 pm
Intial Ecg showing j point elevations in V2,v3,v4 with no reciprocal changes
hyperactue T waves in following Ecgs
With normal sinus rythm and normal axis with rate around 90bpm
Day 3
A 45 yr old male
? TIA
? POTS
? Silent anterior wall MI
? coronary spasm
? Atonic seizures with Todd’s palsy
No fresh complaints
O/e patient conscious, coherent, cooperative.
PR. - on lying 72/min,on standing 96/min
BP. -on lying 120/80,on standing 120/80
CVS. - S1 S2 +
RS. - BAE +
P/A. - Soft, non tender
CUE - Albumin - nil
Sugar. - nil
Pus cells - 3-4
Lipid profile - total cholesterol - 104
Triglycerides- 71
HDL - 42
LDL. - 58
VLDL- 14.2
Sr potassium- 3.9 mmol/l
Psychiatry referral done - working diagnosis - ? Psychosis NOS
RX - TAB LORAZEPAM 2MG / PO/ SOS
Patient was advised for ecg and they want an MRI brain
TREATMENT GIVEN:
INJ OPTINEUROBION 1 AMP IN 100ML NS/IV/TID
INJ PANTOP 40MG/IV/OD
TAB ECOSPRIN AV 75/20MG H/S
Tab CLOPITAB 75mg OD at 8pm


















Comments
Post a Comment